Vitamin C megadosage
Vitamin C megadosage is a term describing the consumption or injection of vitamin C (ascorbate) in doses comparable to the amounts produced by the livers of most other mammals. Such dosages correspond to amounts well beyond the current Dietary Reference Intake. Oral dosages are usually divided and consumed in portions over the day. Injections of hundreds of grams per day are advocated by some physicians for the treatment of certain conditions, poisonings, or recovery from trauma. People who practice vitamin C megadosage may consume many vitamin C pills throughout each day or dissolve pure vitamin C crystals in water or juice and drink it throughout the day.
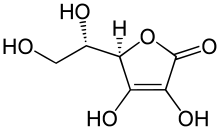
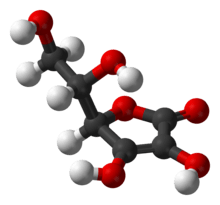
Historic advocates of Vitamin C megadosage include Linus Pauling, who won the Nobel Prize in Chemistry in 1954. Pauling argued that, due to a non-functional form of L-gulonolactone oxidase, an enzyme required to make Vitamin C that is functional in most other mammalian relatives, humans have developed a number of adaptations to cope with the relative deficiency. These adaptations, he argued, ultimately shortened lifespan but could be reversed or mitigated by supplementing humans with the hypothetical amount of vitamin C that would have been produced in the body if the enzyme were working.
Vitamin C megadoses are claimed by alternative medicine advocates including Matthias Rath and Patrick Holford to have preventative and curative effects on diseases such as cancer and AIDS,[1][2] but the available scientific evidence does not support these claims.[3] Some trials show some effect in combination with other therapies, but this does not imply vitamin C megadoses in themselves have therapeutic effect.[4]
Background
The World Health Organization recommends a daily intake of 45 milligrams (mg)/day of vitamin C for healthy adults, and 25–30 mg/day in infants.[5] Vitamin C is necessary for production of collagen and other biomolecules, and for the prevention of scurvy.[6] Vitamin C is an antioxidant, which has led to its endorsement by some researchers as a complementary therapy for improving quality of life.[7] Since the 1930s, when it first became available in pure form, some physicians have experimented with higher than recommended vitamin C consumption or injection.[8] Certain animal species, including haplorhine primates (which includes humans),[9][10] members of the Caviidae family of rodents (including guinea pigs and capybaras),[11] most species of bats,[12] many passerine birds,[13] and about 96% of fish (the teleosts),[13] do not synthesize vitamin C internally.
Since its discovery, vitamin C has been considered almost a panacea by some,[14] although this led to suspicions of it being overhyped by others.[15] Vitamin C has been promoted in alternative medicine as a treatment for the common cold, cancer, polio and various other illnesses. The evidence for these claims is mixed. Orthomolecular-based megadose recommendations for vitamin C are based mainly on theoretical speculation and observational studies, such as those published by Fred R. Klenner from the 1940s through the 1970s. There is a strong advocacy movement for such doses of vitamin C, and there is an absence of large scale, formal trials in the 10 to 200+ grams per day range. The single repeatable side effect of oral megadose vitamin C is a mild laxative effect if the practitioner attempts to consume too much too quickly. A tolerable upper limit (UL) of vitamin C was set at 2 grams for the first time in the year 2000, referencing this mild laxative effect as the reason for establishing the UL.[16]:13
About 70-90% of vitamin C is adsorbed by the body when taken orally at normal levels (30–180 mg daily). Adsorption is only about 50% for daily doses of 1 g. Oral administration, even of mega doses, cannot raise blood concentration above 0.22mM.[17]
Relative deficiency hypothesis

Humans and other species that do not synthesize vitamin C carry a mutated and ineffective form of the enzyme L-gulonolactone oxidase, the fourth and last step in the ascorbate-producing machinery. In the anthropoids lineage, this mutation likely occurred 40 to 25 million years ago. The three surviving enzymes continue to produce the precursors to vitamin C, but the process is incomplete and the body then disassembles them.
In the 1960s, the Nobel-Prize-winning chemist Linus Pauling, after contact[18] with Irwin Stone, began actively promoting vitamin C as a means to greatly improve human health and resistance to disease. His book How to Live Longer and Feel Better was a bestseller and advocated taking more than 10 grams per day orally, thus approaching the amounts released by the liver directly into the circulation in other mammals: an adult goat, a typical example of a vitamin-C-producing animal, will manufacture more than 13,000 mg of vitamin C per day in normal health and much more when stressed.[19]
Matthias Rath is a controversial German physician who worked with and published two articles discussing the possible relationship between lipoprotein and vitamin C with Pauling.[20][21] He is an active proponent and publicist for high-dose vitamin C. Pauling's and Rath's extended theory states that deaths from scurvy in humans during the ice age, when vitamin C was scarce, selected for individuals who could repair arteries with a layer of cholesterol provided by lipoprotein(a), a lipoprotein found in vitamin C-deficient species.[22]
Stone[23] and Pauling[24] believed that the optimum daily requirement of vitamin C is around 2,300 milligrams for a human requiring 2,500 kcal a day.
Pauling criticized the established US Recommended Daily Allowance, pointing out that it is based on the known quantities that will prevent acute scurvy but is not necessarily the dosage for optimal health.[25]
Adverse effects
Although sometimes considered free of toxicity, there are known side effects from vitamin C intake, and it has been suggested that intravenous injections should require "a medical environment and trained professionals."[26]
- A genetic condition that results in inadequate levels of the enzyme glucose-6-phosphate dehydrogenase (G6PD) can cause sufferers to develop hemolytic anemia after using intravenous vitamin C treatment.[27] G6PD deficiency test is a common laboratory test.
- Vitamin C administration may acidify the urine, that could promote the precipitation of kidney stones or drugs in the urine.[26]
- Because oxalic acid is produced in the metabolism of vitamin C, hyperoxaluria can be caused by intravenous administration of ascorbic acid.[26]
Blood levels of vitamin C remain steady at approximately 200 mg per day. Although vitamin C can be well tolerated at doses well above the RDA recommendations, adverse effects can occur at doses above 3 grams per day though overload is unlikely. The common 'threshold' side effect of megadoses is diarrhea. Other possible adverse effects include increased oxalate excretion and kidney stones, increased uric-acid excretion, systemic conditioning ("rebound scurvy"), preoxidant effects, iron overload, reduced absorption of vitamin B12 and copper, increased oxygen demand, and acid erosion of the teeth with chewing ascorbic-acid tablets.[28] In addition, one case has been noted of a woman who had received a kidney transplant followed by high-dose vitamin C and died soon afterwards as a result of calcium oxalate deposits that destroyed her new kidney. Her doctors concluded that high-dose vitamin C therapy should be avoided in patients with renal failure.[29]
Overdose
As discussed previously, vitamin C generally exhibits low toxicity. The LD50 (the dose that will kill 50% of a population) is generally accepted to be 11900 milligrams [11.9 grams] per kilogram in rat populations.[30]
Interactions
Pharmaceuticals designed to reduce stomach acid, such as the proton-pump inhibitors (PPIs), are among the most widely sold drugs in the world. One PPI, omeprazole (Prilosec), has been found to lower the bioavailability of vitamin C by 12% after 28 days of treatment, independent of dietary intake. The probable mechanism of vitamin C reduction, intragastric pH elevated into alkalinity, would apply to all other PPI drugs, though not necessarily to doses of PPIs low enough to keep the stomach slightly acidic.[31] In another study, 40 mg/day of omeprazole lowered the fasting gastric vitamin C levels from 3.8 to 0.7 µg/mL.[32]
Aspirin may also inhibit the absorption of vitamin C.[33][34][35]
Regulation
There are regulations in most countries that limit the claims on the treatment of disease that can be placed on food, drug, and nutrient product labels. Regulations include:
- Claims of therapeutic effect with respect to the treatment of any medical condition or disease are prohibited by the Food and Drug Administration in the US, and by the corresponding regulatory agencies in other countries, unless the substance has gone through a well established clinical trial with neutral oversight.
- In the United States, the following notice is mandatory on food, drug, and nutrient product labels that make health claims: These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.[36]
Research
Cancer
The use of vitamin C in high doses as a treatment for cancer was promoted by Linus Pauling, based on a 1976 study published with Ewan Cameron which reported intravenous vitamin C significantly increased lifespans of patients with advanced cancer.[37][38] This trial was criticized by the National Cancer Institute for being designed poorly, and three subsequent trials conducted at the Mayo Clinic could not replicate these results.[38][39]
More recently, in vitro data in animal models suggests intravenous ascorbic acid at high doses may hold some promise in the treatment of cancer; however, this has not been supported in more rigorous clinical trials in humans. Preliminary clinical trials in humans have shown that it is unlikely to be a "miracle pill" for cancer and more research is necessary before any definitive conclusions about efficacy can be reached.[26] A 2010 review of 33 years of research on vitamin C to treat cancer stated "we have to conclude that we still do not know whether Vitamin C has any clinically significant antitumor activity. Nor do we know which histological types of cancers, if any, are susceptible to this agent. Finally, we don't know what the recommended dose of Vitamin C is, if there is indeed such a dose, that can produce an anti-tumor response."[39]
The American Cancer Society has stated, "Although high doses of vitamin C have been suggested as a cancer treatment, the available evidence from clinical trials has not shown any benefit."[38]
Burns
One study performed in 2000 used high intravenous doses of vitamin C (66 mg/kg/hour over 24 hours, for a total dose of around 110 grams) after severe burn injury,[40] but despite being described as promising, it has not been replicated by independent institutions and thus is not a widely accepted treatment.[41] Based on that study, the American Burn Association (ABA) considers high-dose ascorbic acid an option to be considered for adjuvant therapy in addition to the more accepted standard treatments.[42] However, one medical review article noted vitamin C at the doses studied can be toxic, and recommended further validation by future studies before this therapy is clinically used.[40]
See also
- Ascorbic acid
- Micronutrient
- Macronutrient
- Megavitamin therapy
- Orthomolecular medicine
- Uric acid
- Vitamin
References
- ↑ Bad Science, Ben Goldacre
- ↑ Trick Or Treatment, Simon Singh & Edzard Ernst
- ↑ The Dark Side Of Linus Pauling's Legacy, Quackwatch
- ↑ David Gorski, Science Based Medicine, 18 Aug 2008
- ↑ Vitamin and mineral requirements in human nutrition (PDF) (2nd ed.). World Health Organization. 2004. p. 138. ISBN 9241546123. Retrieved 31 December 2014.
- ↑ Gropper SS, Smith JL, Grodd JL (2004). Advanced Nutrition and Human Metabolism (4th ed.). Belmont, CA. US: Thomson Wadsworth. pp. 260–275.
- ↑ Yeom CH, Jung GC, Song KJ (2007). "Changes of terminal cancer patients' health-related quality of life after high dose vitamin C administration". J. Korean Med. Sci. 22 (1): 7–11. doi:10.3346/jkms.2007.22.1.7. PMC 2693571
 . PMID 17297243.
. PMID 17297243. - ↑ "Vitamin C (Ascorbic Acid)". University of Maryland Medical Center. April 2002. Retrieved 2007-02-19.
- ↑ Pauling L (1970). "Evolution and the need for ascorbic acid". Proc. Natl. Acad. Sci. USA. 67 (4): 1643–1648. Bibcode:1970PNAS...67.1643P. doi:10.1073/pnas.67.4.1643. PMC 283405
 . PMID 5275366.
. PMID 5275366. - ↑ Pollock, J. I.; Mullin, R. J. (1987). "Vitamin C biosynthesis in prosimians: Evidence for the anthropoid affinity of Tarsius". American Journal of Physical Anthropology. 73 (1): 65–70. doi:10.1002/ajpa.1330730106. PMID 3113259.
- ↑ R. Eric Miller; Murray E. Fowler. Fowler's Zoo and Wild Animal Medicine, Volume 8. p. 389. Retrieved 2016-06-02.
- ↑ Jenness R, Birney E, Ayaz K (1980). "Variation of l-gulonolactone oxidase activity in placental mammals". Comparative Biochemistry and Physiology Part B: Biochemistry and Molecular Biology. 67 (2): 195–204. doi:10.1016/0305-0491(80)90131-5.
- 1 2 Martinez del Rio C (July 1997). "Can passerines synthesize vitamin C?". The Auk. 114 (3): 513–16. doi:10.2307/4089257. JSTOR 4089257.
- ↑ Levy, Thomas (2011). Primal Panacea. MedFox Publishing. p. 352. ISBN 0983772800.
- ↑ Harri Hemilä (January 2006). "Do vitamins C and E affect respiratory infections?" (PDF). University of Helsinki. Retrieved 2007-02-21.
- ↑ Institute of Medicine. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, DC: The National Academies Press, 2000.
- ↑ "Office of Dietary Supplements - Vitamin C". ods.od.nih.gov. Retrieved 2016-02-26.
- ↑ "My Love Affair with Vitamin C" (PDF).
- ↑ Stone, I. (1979). "Homo sapiens ascorbicus, a biochemically corrected robust human mutant". Medical Hypotheses. 5 (6): 711–721. doi:10.1016/0306-9877(79)90093-8. PMID 491997.
- ↑ Rath M, Pauling L (1990). "Immunological evidence for the accumulation of lipoprotein(a) in the atherosclerotic lesion of the hypoascorbemic guinea pig". Proc Natl Acad Sci USA. 87 (23): 9388–9390. Bibcode:1990PNAS...87.9388R. doi:10.1073/pnas.87.23.9388. PMC 55170
 . PMID 2147514.
. PMID 2147514. - ↑ Rath M, Pauling L (1990). "Hypothesis: lipoprotein(a) is a surrogate for ascorbate". Proc. Natl. Acad. Sci. USA. 87 (16): 6204–6207. Bibcode:1990PNAS...87.6204R. doi:10.1073/pnas.87.16.6204. PMC 54501
 . PMID 2143582.
. PMID 2143582. - ↑ Rath M, Pauling L (1992). "A unified theory of human cardiovascular disease leading the way to the abolition of this disease as a cause for human mortality" (PDF). Journal of Orthomolecular Medicine. 7 (1): 5–15.
- ↑ Stone, Irwin (1972). The Healing Factor: Vitamin C Against Disease. Grosset and Dunlap. ISBN 0-448-11693-6. OCLC 3967737.
- ↑ Pauling, Linus (1970). "Evolution and the need for ascorbic acid". Proc. Natl. Acad. Sci. USA. 67 (4): 1643–1648. Bibcode:1970PNAS...67.1643P. doi:10.1073/pnas.67.4.1643. PMC 283405
 . PMID 5275366.
. PMID 5275366. - ↑ Pauling, Linus (1986). How to Live Longer and Feel Better. W. H. Freeman and Company. ISBN 0-380-70289-4. OCLC 154663991.
- 1 2 3 4 Verrax J, Calderon PB (December 2008). "The controversial place of vitamin C in cancer treatment". Biochem. Pharmacol. 76 (12): 1644–52. doi:10.1016/j.bcp.2008.09.024. PMID 18938145.
- ↑ Rees; Kelsey, Richards (March 1993). "Acute haemolysis induced by high dose ascorbic acid in glucose-6-phosphate dehydrogenase deficiency" (PDF). British Medical Journal. 306 (6881): 841–2. doi:10.1136/bmj.306.6881.841. PMC 1677333
 . PMID 8490379.
. PMID 8490379. - ↑ Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids: a report of the Panel on Dietary Antioxidants and Related Compounds, Subcommittees on Upper Reference Levels of Nutrients and of Interpretation and Use of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Washington, D.C: National Academy Press. 2000. pp. 156–161. ISBN 0-309-06949-1.
- ↑ Nankivell, BJ; Murali KM (2008). "Renal failure from vitamin C after transplantation" (PDF). The New England Journal of Medicine. 358 (4): e4. doi:10.1056/NEJMicm070984. PMID 18216350.
- ↑ "Safety (MSDS) data for ascorbic acid". Oxford University. October 9, 2005. Retrieved 2007-02-21.
- ↑ E. B. Henry, A. Carswell, A. Wirz, V. Fyffe & K. E. L. Mccoll (September 2005). "Proton pump inhibitors reduce the bioavailability of dietary vitamin C". Alimentary Pharmacology & Therapeutics. Retrieved 2007-02-21.
- ↑ C. Mowat; A. Carswell; A. Wirz; K.E. McColl (April 1999). "Omeprazole and dietary nitrate independently affect levels of vitamin C and nitrite in gastric juice.". Alimentary Pharmacology & Therapeutics. Retrieved 2011-02-14.
- ↑ Loh HS, Watters K & Wilson CW (1 November 1973). "The Effects of Aspirin on the Metabolic Availability of Ascorbic Acid in Human Beings". J Clin Pharmacol. 13 (11): 480–486. doi:10.1002/j.1552-4604.1973.tb00203.x. PMID 4490672.
- ↑ Basu TK (1982). "Vitamin C-aspirin interactions". Int J Vitam Nutr Res Suppl. 23: 83–90. PMID 6811490.
- ↑ Ioannides C, Stone AN, Breacker PJ & Basu TK (1982). "Impairment of absorption of ascorbic acid following ingestion of aspirin in guinea pigs". Biochem Pharmacol. 31 (24): 4035–4038. doi:10.1016/0006-2952(82)90652-9. PMID 6818974.
- ↑ "Dietary Supplement Health and Education Act of 1994".
- ↑ Cameron E, Pauling L (October 1976). "Supplemental ascorbate in the supportive treatment of cancer: Prolongation of survival times in terminal human cancer". Proc. Natl. Acad. Sci. USA. 73 (10): 3685–3689. Bibcode:1976PNAS...73.3685C. doi:10.1073/pnas.73.10.3685. PMC 431183
 . PMID 1068480.
. PMID 1068480. - 1 2 3 "Vitamin C". American Cancer Society.
- 1 2 Cabanillas, F (2010). "Vitamin C and cancer: what can we conclude--1,609 patients and 33 years later?". Puerto Rico Health Sciences Journal. 29 (3): 215–7. PMID 20799507.
- 1 2 Berger MM (October 2006). "Antioxidant micronutrients in major trauma and burns: evidence and practice". Nutr Clin Pract. 21 (5): 438–49. doi:10.1177/0115426506021005438. PMID 16998143.
- ↑ Greenhalgh DG (2007). "Burn resuscitation". J Burn Care Res. 28 (4): 555–65. doi:10.1097/bcr.0b013e318093df01. PMID 17665515.
- ↑ Pham TN, Cancio LC, Gibran NS (2008). "American Burn Association practice guidelines burn shock resuscitation". J Burn Care Res. 29 (1): 257–66. doi:10.1097/BCR.0b013e31815f3876. PMID 18182930.
External links
- Quackwatch article critical of megadosing for cold prevention, Charles W. Marshall, Ph.D. Accessed 2016-06-02.