Timeline of healthcare in India
This is a timeline of healthcare in India. Major events such as crises, policies and organizations are included.
Big picture
| Year/period | Key development |
|---|---|
| Prehistory | The knowledge of the medicinal value of plants and other substances and their uses goes back to the time of the earliest settlers. Medical knowledge evolves through trial and error and exchange of know-how between diverse communities and regions.[1] |
| Traditional medicine period | Ayurveda, the science of life, has been the traditional system of healthcare in India for more than 5000 years. This medical system is well-established around 2500 to 600 BC, when it evolves into 2 schools: the School of Physicians and the School of Surgeons.[2] |
| 1600–1947 | British colonial period. East India Company is established. Many British physicians assume broader scholarly roles and European medicine comes to be looked upon as the dominant medical knowledge system. British official colonial policy marginalizes indigenous medicine to secondary status. Notwithstanding European medicine becomes the official health care system, Ayurvedic colleges are still created. Ayurveda education becomes integrated with western concepts of healthcare.[1] |
| 1947 onward | Post-independence period. The government of India makes efforts to recognize Ayurveda, Siddha and Unani as being on par with scientific medicine. Nevertheless, the general trend increasingly complies with the norms of modern medicine. In traditional medical schools the vocabulary and diagnostic tools of modern medicine replace traditional terms and techniques, and students increasingly become unfamiliar with classical references and methodologies.[1] |
| 1980 onward | Numerous government subsidies allow the introduction of private health providers. Also opening up of the market in the 90s further gives impetus to the development of the private health sector in India.[3] Immunization programs increase. |
| 21st century | Today, the health status of India is still on a developing level. The private sector is the dominant healthcare provider. Private chains of healthcare providers are innovating very rapidly, offering high quality treatment at very low cost. As India incorporates world class technology and training, and low cost of service, a trend of medical tourism develops and strengthens in the 2010s.[4][5] |
Full timeline
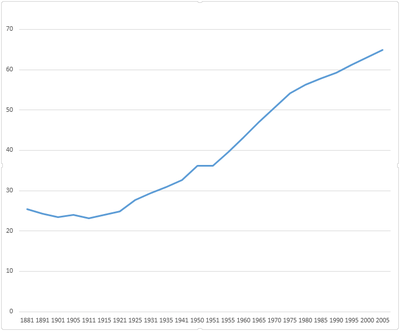
Evolution of life expectancy in India for period between 1881 and 2005.[6]
| Year/period | Type of event | Event | Location |
|---|---|---|---|
| 7000 BCE | Origin | Medical interventions such as dentistry and trepanation are practiced as early as this time.[1] | Indian subcontinent |
| 5000 BCE | Development | Origin of Ayurveda medicine, when it originates as an oral tradition.[7][8] | |
| 2500–1700 BCE | Development | Origin of Siddha medicine.[9] | Tamilakam |
| 600 BCE | Development | Ayurveda is branched into internal medicine; pediatrics; psychiatry; surgery; eye, ear, nose, and throat; toxicology; geriatrics; and eugenics/aphrodisiacs. | |
| 8th century CE | Development | Texts called Nighantus dealing exclusively with the materia medica of Ayurveda are composed. Many of these works help to enlarge the repertoire of medicinal substances by incorporating knowledge of local practitioners and from foreign sources. A few well-known Nighantus are Madanapala Nighantu, Bhavaprakasha Nighantu, Dhanvantari Nighantu and Sodhala Nighantu.[1] | |
| 1200s | Development | Unani medicine system is introduced in India via Rome. It integrates with other systems such as Ayurveda and Yoga.[10] | |
| 1600s | Development | Introduction of western medicine in India. First medical officers arrive along with the British East India Company's first fleet as ship's surgeons.[11] | |
| 1664 | Organization (hospital) | The Madras General Hospital is the first hospital opened in India.[11][12] | Chennai |
| 1707 | Organization (hospital) | The Presidency General Hospital is formed.[11][13] | Calcutta |
| 1802 | Organization (government body) | A Superintendent General of Vaccination in India is appointed after the discovery of the smallpox vaccine.[11] | |
| 1817 | Crisis | First cholera pandemic originates in the Ganges River Delta.[14] | |
| 1823 | Organization (medical school) | The Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER) is founded. It's the oldest to teach European medicine in Asia. Today considered an Institute of National Importance.[15][16][17] | Pondicherry |
| 1829 | Crisis | Second cholera pandemic originates in the Ganges River Delta.[14] | |
| 1835 | Organization (medical school) | The Calcutta Medical College is established.[11] | Calcutta |
| 1852 | Crisis | Third cholera pandemic originates in the Ganges River Delta.[14] | |
| 1854 | Development | The government of India agrees to supply medicines and instruments to the growing network of minor hospitals and dispensaries. Government Store Depots are established in cities.[11] | Calcutta, Madras, Bombay, Mian Mir, and Rangoon. |
| 1858 | Organization (asylum) | Lunate asylums are established for insane persons.[11] | |
| 1860 | Organization (medical school) | The Lahore Medical School is established.[11] | Lahore (now in Pakistan) |
| 1863 | Crisis | Fourth cholera pandemic originates in the Ganges River Delta.[14] | |
| 1869 | Development | A Public Health Commissioner and a Statistical Officer are appointed to the Government of India.[11] | |
| 1870 | Organization (government body) | A central sanitary department is formed.[11] | |
| 1873 | Policy | The Birth and Death Registration Act is passed.[11] | |
| 1880 | Policy | An act is passed for the compulsory vaccination of children in municipalities and cantonments. Smallpox is the main target during this period, although vaccinations are also carried out for plague and other diseases.[11] | |
| 1881 | Crisis | Fifth cholera pandemic originates in India.[14] | Bengal |
| 1896 | Organization (government body) | The Plague Commission is constituted.[11] | |
| 1896 | Crisis | The Bombay plague epidemic breaks out. It spreads across all of India and kills at least 2 million people.[11] | |
| 1897 | Policy | The Epidemic Diseases Act is passed. The Governor General of India confers special powers upon local authorities to implement the necessary measures for control of epidemics.[11] | |
| 1899 | Crisis | Sixth cholera pandemic originates in India.[14] | |
| 1912 | Organization (government body) | The Government of India sanctions the appointment of Deputy Sanitary Commissioners and Health Officers with the local bodies and releases funds for sanitation.[11] | |
| 1912 | Policy | The Indian Lunacy Act is passed.[18] | |
| 1925 | Organization (medical institution) | The National Institute of Mental Health and Neurosciences is established. Today listed as an Institute of National Importance.[15][19] | Bangalore |
| 1930 | Organization (health training) | The All-India Institute of Hygiene and Public Health is established.[11] | Calcutta |
| 1933 | Policy | The Medical Council of India is formed, with the purpose of establishing uniform and high standards of medical education in India.[18] | |
| 1938 | Policy | The Bombay Medical Practitioner's Act is passed. With it comes the first legal recognition and registration for the Indian systems of medicine.[18] | |
| 1939 | Organization (health training) | The first Rural Health Training Center is established near Calcutta.[11] | Singur |
| 1939 | Organization | The Tuberculosis Foundation of India is established.[11] | |
| 1940 | Policy | The Drugs Act is passed and drugs are made under the control of the government for the first time.[11] | |
| 1948 | Program launch (healthcare coverage) | The Employees' State Insurance Scheme (ESIS) is launched with the objective of achieving universal health coverage. Targeted at employees with income less than Rs 15000/month and dependents.[20] | |
| 1950 | Policy | The Insurance Amendment Act leads to the Government of India deciding to nationalize the insurance business.[20] | |
| 1953 | Organization (hospital chain, medical school chain) | Manipal Hospitals is founded as a part of the Manipal Education and Medical Group (MEMG).[21] | Bangalore |
| 1953 | Policy | The Delhi Nursing Home Registration Act is passed.[18] | Delhi |
| 1954 | Program launch (healthcare coverage) | The Central Government Health Scheme (CGHS) is launched with the objective of achieving universal health coverage in government employees and families.[20] | |
| 1956 | Organization (medical college chain) | The All India Institutes of Medical Sciences (AIIMS) are founded with a first college in New Delhi. These institutes are declared institute of national importance by the Act of Parliament.[15] | New Delhi |
| 1962 | Organization (medical and research institution) | The Postgraduate Institute of Medical Education and Research is established. Today listed as an institute of national importance.[15] | Chandigarh |
| 1964 | Organization (government body) | A government body for setting norms for the manufacture and the control of the quality of traditional medicinal preparations is formed.[1] | |
| 1970 | Program launch (nutrition) | The Government of India launches the Balwadi Nutrition Programme to provide food supplements at Balwadis to children of the age group 3–6 years in rural areas.[22][23] | |
| 1970 | Policy | The government of India passes the Indian Medical Central Council Act to standardize Ayurvedic teaching institutions, their curriculum and their diplomas.[1] | |
| 1975 | Program launch (nutrition, child health) | The Integrated Child Development Services (ICDS) scheme is launched with the purpose of improving nutrition and health status in children.[20] | |
| 1976 | Organization (hospital chain) | Aravind Eye Hospitals chain is opened by Dr. Govindappa Venkataswamy as a network of eye hospitals. Having a major impact in eradicating cataract related blindness in India, today the model of Aravind Eye Care hospitals is highly recognized and has won multiple awards.[24][25][26] | Tamil Nadu, Madurai, Theni, Tirunelveli, Coimbatore, Pondicherry, Dindigul, Tirupur, Salem, Tuticorin, Udumalpet. |
| 1983 | Policy | The National Health Policy is endorsed by the Parliament of India.[27] | |
| 1983 | Organization (hospital chain) | Apollo Hospitals opens its first facility. It is the first hospital to be registered as a publicly listed company in India.[21] | Chennai |
| 1985 | Program launch (immunization) | The government of India launches the Universal Immunization Programme, consisting in massive vaccination for nine diseases: tuberculosis, diphtheria, pertussis (whooping cough), tetanus, poliomyelitis, measles, Hepatitis B, Diarrhoea, Japanese Encephalitis and Pneumonia.[28][29] | |
| 1990 | Organization (hospital) | Pharmaceutical company Wockhardt opens its first medical center.[21] | Kolkata |
| 1994 | Crisis | 1994 plague. Bubonic and pneumonic plague break out.[30] | South-central and southwestern India |
| 1994 | Crisis | Pneumonic plague epidemic in Surat breaks out.[31] | Gujarat |
| 1995 | Organization (government body) | The Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH) is created as a governmental body in India purposed with developing education and research in ayurveda, yoga, naturopathy, unani, siddha, homeopathy, and other alternative medicine systems.[1] | |
| 1995 | Program launch (immunization) | Pulse Polio program is launched by the government to eradicate poliomyelitis by vaccinating all children under the age of five years.[32] | |
| 1996 | Organization (hospital chain) | Fortis Healthcare is founded.[21] | Delhi |
| 1997 | Program launch (immunization) | The Revised National Tuberculosis Control Program (RNTCP) is launched by the government with aims at achieving universal access to tuberculosis control services.[33] | |
| 2000 | Policy (healthcare coverage) | The Insurance Regulatory and Development Act (IRDA) opens up the market with the invitation for registration applications.[20] | |
| 2000 | Organization | The Krishna Heart Institute is founded as a high-end medical facility, specializing in heart diseases.[34] | Ahmedabad, India |
| 2000 | Report | The World Health Organization's global healthcare profile ranks India’s healthcare system 112th out of 190 countries.[20] | |
| 2000 | Organization (medical school) | The Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST) is established. Listed as an Institute of National Importance[15] | Thiruvananthapuram |
| 2000–present | Organization (hospital chain) | Narayana Health system is opened as a multi-specialty hospital chain by Dr. Devi Shetty under the guidance of the Asian Heart Foundation. Today it has 31 hospitals in 19 locations. It is one of India's largest and considered the world's most economical[35] healthcare providers with a reputation for high quality.[36][37] | Bengaluru, Ahmedabad, Davangere, Dharwad, Bellary, Berhampore, Jaipur, Jamshedpur, Katra, Kolar, Kolkata, Mahuva, Mysore, Palanpur, Raipur, Shimoga, Durgapur, Guwahati. |
| 2002–2005 | Program launch (lifestyle diseases) | The Tobacco cessation clinic program (later renamed as Tobacco Cessation Centers) is launched by the World Health Organization (WHO) and the Ministry of Health of India. Until 2005, 18 facilities are created. The services offered at the clinics include individual intervention in the form of behavioral counseling, medication, and nicotine replacement therapy[38] | Anand, Bhopal, Bangalore, Chandigarh, Chennai, Cuttack, Delhi, Goa, Jaipur, Lucknow, Mumbai, and Patna, Mizoram, Guwahati, Kolkata, Hyderabad and Trivandrum |
| 2004 | Program launch (healthcare coverage) | The Deen Dayal Antyoday Upchar Yojna scheme is launched by the government of Madhya Pradesh to provide free health care to poor families.[39] | Madhya Pradesh |
| 2005 | Program launch (healthcare coverage) | The National Rural Health Mission (NRHM) is launched by the government of India.[40] | |
| 2005 | Program launch (healthcare coverage) | Accredited Social Health Activist (ASHAs) is launched as a program of community health workers instituted by the Ministry of Health and Family Welfare.[41] | |
| 2005 | Program launch (child mortality) | The Janani Suraksha Yojana scheme is launched by the Government of India with aims at decreasing the neonatal and maternal deaths happening in the country by promoting institutional delivery of babies.[42] | |
| 2007 | Program launch (healthcare coverage) | The Government of Andhra Pradesh launches the Aarogyasri program in order to provide no cost coverage of hospitalization for all those below the poverty line.[43] | Andhra Pradesh |
| 2009 | Program launch (healthcare coverage) | The Rashtriya Swasthya Bima Yojana (RSBY) scheme is launched with the objective of providing affordable healthcare to the poor.[20] | |
| 2011 | Program launch (healthcare coverage) | The National Programme for the Health Care of the Elderly (NPHCE) scheme is launched with the objective of providing the elderly an easy access to primary healthcare.[20] | |
| 2012 | Organization (medical college chain) | All India Institute of Medical Sciences expand to six locations.[44] | Bhopal, Bhubaneswar, Jodhpur, Patna, Raipur and Rishikesh. |
| 2014 | Crisis | Odisha jaundice outbreak. Mainly Hepatitis E and also Hepatitis A kill at least 36 people.[45] | Odisha, Bolangir district, Cuttack, Khurda and Jajpur |
| 2014 | Program launch (immunization) | Mission Indradhanush is launched by the Ministry of Health and Family Welfare with the purpose of immunizing all children against seven vaccine preventable diseases, namely diphtheria, pertussis, tetanus, polio, tuberculosis, measles and hepatitis B by 2020.[46] | |
| 2014 | Program launch (immunization) | TB-Mission 2020 is launched by the Government of India with the purpose of eliminating tuberculosis from the country in 2020.[47] | |
See also
References
- 1 2 3 4 5 6 7 8 "OVERVIEW OF INDIAN HEALING TRADITIONS".
- ↑ Mishra L, Singh BB, Dagenais S. "Ayurveda, a historical perspective and principles of the traditional healthcare system in India.". PubMed. PMID 11253415.
- ↑ Baru,Rama V(2010): “Public Sector Doctors in an Era of Commercialisation” in Sheikh and A George(ed)Health Providers in India, on the Frontlines of Change(New Delhi: Routledge)81-96.
- ↑ Amit Sengupta. "The private health sector in India". doi:10.1136/bmj.331.7526.1157. PMC 1285083
 .
. - ↑ "Favorable exchange rate boost the medical tourism industry: MRRSE".
- ↑ "Life expectancy". Retrieved 19 November 2016.
- ↑ T.S.S. Dikshith (2008). Safe Use of Chemicals: A Practical Guide. CRC Press. p. 16.
- ↑ Elizabeth R. Mackenzie; Birgit Rakel (2006). Complementary and Alternative Medicine for Older Adults: A Guide to Holistic Approaches to Healthy Aging. Springer. p. 215. ISBN 9780826138064.
- ↑ "Siddha".
- ↑ "About Unani".
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Muhammad Umair Mushtaq. "Public Health in British India: A Brief Account of the History of Medical Services and Disease Prevention in Colonial India". US National Library of Medicine. doi:10.4103/0970-0218.45369. PMC 2763662
 .
. - ↑ "Government General Hospital".
- ↑ "Presidency General Hospital".
- 1 2 3 4 5 6 "Cholera pandemics".
- 1 2 3 4 5 "Institutions of national importance".
- ↑ History & Milestones. JIPMER. Retrieved on 2013-10-09.
- ↑ B'lore: NIMHANS gets national importance status - News Oneindia. News.oneindia.in (2010-10-21). Retrieved on 2013-10-09.
- 1 2 3 4 "Regulations In Hospital & Healthcare In India". Retrieved 26 September 2016.
- ↑ "National Institute of Mental Health and Neurosciences".
- 1 2 3 4 5 6 7 8 "Healthcare in India" (PDF).
- 1 2 3 4 "Hospital Chains in India:The Coming of Age?".
- ↑ "Balwadi Nutrition Programme". National Institute of Health and Family Welfare. Retrieved 20 November 2012.
- ↑ "Important programmes to combat malnutrition in India". Food and Agricultural Organisation. Retrieved 20 November 2012.
- ↑ "About Aravind Eye Hospitals".
- ↑ "An Infinite Vision: The Story of Aravind Eye Hospital".
- ↑ "A Hospital Network With a Vision".
- ↑ Jugal Kishore (2005). National health programs of India: national policies & legislations related to health. Century Publications. ISBN 978-81-88132-13-3. Retrieved 2 September 2012.
- ↑ "Immunization programme" (PDF).
- ↑ Patra, Nilanjan. "UNIVERSAL IMMUNIZATION PROGRAMME IN INDIA: THE DETERMINANTS OF CHILDHOOD IMMUNIZATION" (PDF). Indian Statistical Institute, Calcutta. p. 1. Retrieved 1 February 2012.
- ↑ "International Notes Update: Human Plague—India, 1994". MMWR Morb. Mortal. Wkly. Rep. 43 (41): 761–762. 21 October 1994. PMID 7935308. Retrieved 26 December 2015.
- ↑ Dutt, Ashok (July 2006). "Surat Plague of 1994 Re-Examined" (PDF). Review. 37 (4): 755–760. Retrieved 31 October 2015.
- ↑ "pulse polio".
- ↑ National Strategic Plan for Tuberculosis Control, 2012-2017 (PDF). Central TB Division, Ministry of Health and Family Welfare. Aug 2012. Retrieved 22 November 2015.
- ↑ "Krishna Heart Institute". Retrieved 31 July 2016.
- ↑ "Narayana Multispeciality Hospital".
- ↑ "Philanthropy Awards 2013". Online webpage of Forbes India. Retrieved 2013-12-06.
- ↑ "Quality, affordability and scale in healthcare: learning from Narayana". Online webpage of The Health Foundation Inspiring Improvement. Retrieved 2013-12-06.
- ↑ K. R. Thankappan. "Tobacco cessation in India: A priority health intervention". PMC 4078486
 .
. - ↑ "Deen Dayal Antyoday Upchar Yojna".
- ↑ Umesh Kapil and Panna Choudhury National Rural Health Mission (NRHM): Will it Make a Difference? Indian Pediatrics Vol. 42 (2005): 783
- ↑ ASHA, Ministry of Health and Family Welfare (MoHFW), 2005
- ↑ "National Health Mission, Government of India". Retrieved 11 March 2015.
- ↑ "Toward Universal Hospital Coverage: The Aarogyasri Health Insurance Program of Andhra Pradesh".
- ↑ "New All India Institutes of Medical Sciences".
- ↑ "Jaundice Resurfaces, Claims 2 More". The New Indian Express. 3 January 2014. Retrieved 7 January 2015.
- ↑ "Mission Indradhanush".
- ↑ Dr Harsh Vardhan announces India’s “TB-Mission 2020”
This article is issued from Wikipedia - version of the 11/19/2016. The text is available under the Creative Commons Attribution/Share Alike but additional terms may apply for the media files.