Respiratory examination
In medicine, the respiratory examination is performed as part of a physical examination,[1] or when a patient presents with a respiratory problem (dyspnea (shortness of breath), cough, chest pain) or a history that suggests a pathology of the lungs. It is very rarely performed in its entirety or in isolation; most commonly, it is merged with the cardiac examination.
Positioning and environment
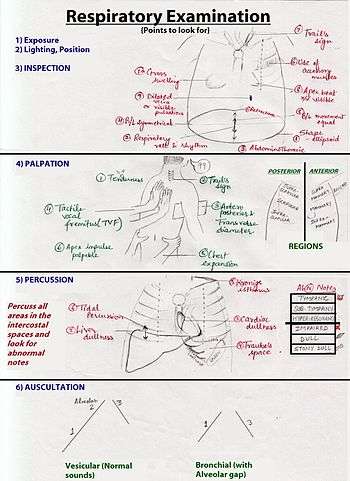
In the respiratory examination, the patient is asked to sit upright on an examination table, with arms at the side. Adequate lighting is ensured and the patient is asked to expose his or her chest.
Later in the examination, when the back is examined, the patient is usually asked to move the arms forward so that the scapulae are not in the way of examining the upper lung fields. These fields are intended to correlate with the lung lobes and are thus tested on the anterior and posterior chest walls (the front and back of the patient's thorax).
The respiratory exam has conventionally been split into different stages:
- Position of the person and the environment.
- Inspection of the person and respiratory effort.
- Palpation of the person's anterior and posterior chest.
- Percussion of the person's anterior and posterior chest walls.
- Auscultation of the person's anterior and posterior chest walls.
One method to remember the steps of the examination is through the mnemonic PIPPA:
When accompanying other physicians or students, medical staff typically report as they examine a patient. Examples of a normal examination may include:
- adjustment of environment
- "on inspection, effort is normal"
- "no tenderness to palpation", "fremitus WNL (within normal limits)"
- "clear to percussion bilaterally" or "CTP B"
- "clear to auscultation bilaterally" or "CTA B"; "no R/R/W (rhonchi, rales or wheezes)"
Inspection
The examiner then observes the patient's respiratory rate, which is typically conducted under the pretext of some other exam, so that patient does not subconsciously increase their baseline respiratory rate. Signs of respiratory distress may include:
- Cyanosis, a bluish tinge of the extremities (peripheral cyanosis), or of tongue (central cyanosis).
- Pursed-lip breathing
- Accessory muscle use,including the scalene and intercostal muscles.
- Diaphragmatic breathing, paradoxical movement of the diaphragm outwards during inspiration.
- Intercostal indrawing.
- Decreased chest–chest movement on the affected side.
- An increased jugular venous pressure, indicating possible right heart failure
Chest wall abnormalities are also examined, and may include:
- Kyphosis, abnormal anterior-posterior curvature of the spine
- Scoliosis, abnormal lateral curvature of the spine
- Barrel chest, - chest wall increased anterior-posterior; normal in children; typical of hyperinflation seen in COPD
- Pectus excavatum - sternum sunken into the chest
- Pectus carinatum - sternum protruding from the chest
As well as the patient's respiratory rate, the pattern of breathing is also noted:
- An acidotic patient will have more rapid breathing to compensate, known as Kussmaul breathing.
- Cheyne–Stokes respiration, which is alternating breathing in high frequency and low frequency from brain stem injury. It can be seen in newborn babies which is sometimes physiological (normal). Also observe for retractions seen in asthmatics. Retractions can be supra-sternal, where the accessory muscles of respirations of the neck are contracting to aid inspiration. Retractions can also be intercostal, in which there is visible contraction of the intercostal muscles (between the ribs) to aid in respiration. These are signs of respiratory distress.
The physician then typically inspects the fingers for cyanosis and clubbing.
Tracheal deviation is also examined.
Palpation
The physician then places both palms on the posterior lung fields, asking the patient to count 1 to 10. The physician aims to feel for vibrations and compare the right/left lung fields. If the patient has a consolidation, (for example caused by pneumonia), the vibration will be louder at that part of the lung. This is because sound travels faster through denser material than air.
If a patient has pneumonia, palpation may reveal increased vibration and dullness on percussion. If there is pleural effusion, palpation should reveal decreased vibration and there will be 'stony dullness' on percussion.
The examiner then tests for
- Tracheal deviation, whether trachea is in centred or not, indicating enlargement or collapse of a lung field.
- Tactile fremitus, with the patient asked to say boy-O-boy or ninety-nine, and the physician using the ulnar aspect of their hand to feel changes in sound conduction.
- Respiratory expansion, indicating whether lung expansion is equal.
- the position of the apex beat to check if there has been deviation of the heart.
Percussion
The physician attempts to examine changes in density of the lung fields by examining its resonance.
Specifically, percussion is performed with the middle finger striking the middle phalanx of the other middle finger of the other hand. The sides of the chest are compared. This is performed symmetrically on all lung fields, on the anterior and posterior chest walls.
Examples of alterations in density may include pleural effusion and pneumothorax. The sound is described as tympanic if there is a pneumothorax because air will stretch the pleural membranes. Conversely, if there is fluid between the pleural membranes, the percussion will be dampened and sound muffled.
- dullness indicates consolidation
- hyper-resonance (as can be simulated by percussing the inflated cheek) suggests a pneumothorax (can be related to COPD or a pleural effusion)
- diaphragmatic excursion - normal is 3 to 6 cm.
Auscultation
[2] The physician then auscultates the respiratory sounds over the lung fields, listening to the fields through a stethoscope. This is conducted while the patient is breathing, noting normal breath sounds and any abnormalities including:
- Wheezes, describing a continuous musical sound on expiration or inspiration. A wheeze is the result of narrowed airways. Common causes include asthma and emphysema
- Rhonchi (an increasingly obsolete term) characterised by low pitched, musical bubbly sounds heard on inspiration and expiration. Rhonchi are the result of viscous fluid in the airways.
- Crackles or rales. Intermittent, non-musical and brief sounds heard during inspiration only. They may be described as fine (soft, high-pitched) or coarse (louder, low-pitched). These are the result of alveoli opening due to increased air pressure during inspiration. Common causes include congestive heart failure.
- Stridor a high-pitched musical breath sound resulting from turbulent air flow in the larynx or lower in the bronchial tree. It is not to be confused with stertor. Causes are typically obstructive, including foreign bodies, croup, epiglottitis, tumours, infection and anaphylaxis.
- Appropriate ratio of inspiration to expiration time (expiration time increased in COPD)
- Bronchial or vesicular breath sounds.
Lastly an assessment of transmitted voice sounds is performed.
References
- ↑ Colin D. Selby (25 October 2002). Respiratory : an illustrated colour text Check
|url=value (help). Elsevier Health Sciences. pp. 14–. ISBN 978-0-443-05949-0. Retrieved 7 March 2011. - ↑ Palaniappan R, Sundaraj K, Ahamed NU, Arjunan A, Sundaraj S. Computer-based Respiratory Sound Analysis: A Systematic Review. IETE Tech Rev 2013;30:248-56
External links
- Respiratory exam - University of Florida
- Exam of the chest - University of Florida
- Respiratory exam - Respiratory Exam
- Lung sounds online - Emory University School of Medicine